Events
Latest | Home | About | Our People | CLAFH | Events | News | Stories | IPS Affiliates | Training
Special Event
HELP LAUNCH A NATIONAL MOVEMENT TO ELIMINATE HEALTH INEQUITIES!
December 17, 12-2pm ET
Join the launch of a bold national campaign, be first to see IPS National Health Inequities Survey results and hear experts turn insights into action.
IPS invites you to the launch of Bridging Our Divide—a bold new campaign to confront the systemic and structural health inequities that harm the health of the country.
Presented in-person and virtually, this special event features the release of findings from the inaugural IPS National Health Inequities Survey. This groundbreaking annual survey is the first of its kind to measure how Americans across diverse populations view and experience health inequities.
Moderated by IPS Executive Director, Dr. Vincent Guilamo-Ramos, a distinguished panel of health and policy experts including Dr. Sylvia Trent-Adams, Dr. Steven Woolf, and Dr. Gregg Gonsalves will unpack the Survey results and explore how they can drive actions that effectively eliminate health inequities and repair our broken health systems.
In these divisive times, this campaign offers a rare opportunity to be part of a uniting force-building bridges to a healthier nation for all.
Register now and add your voice to the movement!
Speakers

Vincent Guilamo-Ramos,
PhD, RN, FAAN
Executive Director, IPS: Professor, Johns Hopkins School of Nursing

Sylvia Trent-Adams,
PhD, RN, FAAN
President and CEO, Institute for Healthcare Improvement

Steven Woolf
MD, MPH
Professor, VCU School of Medicine; Senior Fellow, Center for American Progress
Gregg Gonsalves,
PhD
Associate Professor, Yale School of Public Health; Public Health Correspondent, The Nation

IPS Student
Open House
Oct. 14, 2025, 3-4 PM ET

Past Events
View past event
information from IPS.
IPS STudent Open House – Oct. 14, 2025, 3-4 PM ET
VIRTUAL-only event*
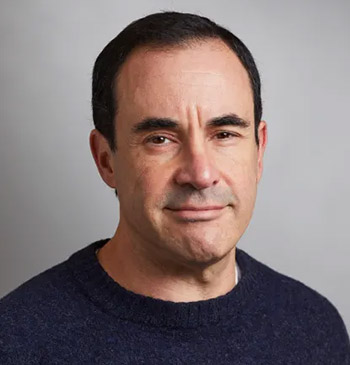
The next IPS Student Open House will be hosted in partnership with CLAFH and the JHSON Office of Admissions as part of the Dimensions of Nursing Virtual Information Session series for students. Register now to learn more about our mission to eliminate health care and health inequities!
On Tuesday, Oct. 14, 3-4 p.m. ET, the JHSON Office of Admissions’ Dimensions of Nursing series, in partnership with the School’s Institute for Policy Solutions (IPS) and the Center for Latino Adolescent and Family Health (CLAFH), will spotlight the aligning work of IPS and CLAFH, devoted to eliminating health inequities as the most promising fix for our broken U.S. health system—and to deliver optimal health outcomes for all by drawing on the wisdom, expertise, and leadership of nurses. Alexander Murphy, assistant director of admissions and recruitment, JHSON, will facilitate a discussion with Professor Vincent Guilamo-Ramos, PhD, RN, FAAN, IPS Executive Director, and CLAFH founding director.
To attend this virtual open house, click “Register Now” below. Please send any questions to [email protected].
*Please note: If you registered for this event before Sept. 24, 2025, details may have changed. A member of the IPS team will be in contact to assist you.
Past Events
NURSING SCIENCE INCUBATOR FOR SOCIAL DETERMINANTS OF HEALTH (SDOH) SOLUTIONS (N-SISS)
October 2, 2025 – Development of A Statistical Analysis Plan
Subhash Aryal, PhD joined the School of Nursing at Johns Hopkins University in 2024. He serves as the Director of Biostatistics and Methods Core at the School of Nursing. Most recently, he was the Director of BECCA Lab in the School of Nursing at University of Pennsylvania. Dr. Aryal conducts both statistical theoretical and interdisciplinary research. His methodological research focuses on developing statistical methods for groundwater monitoring, sample size calculation and treatment of zero-inflated data.
As a public health professional Dr. Aryal is focused on reducing health disparities by addressing barriers to accessing health care. His collaborators include medical professionals, bench scientists and public health researchers conducting research on sleep disorder, HIV/AIDS and chronic pain. He serves on the editorial board of journal “Anesthesiology” as a statistical editor.

Subhash Aryal, PhD
September 23, 2025 – New Update: NIH Study Sections Review Criteria
Alida Bouris is an Associate Professor at the University of Chicago Crown Family School ofSocial Work, Policy, and Practice, and Co-Director of the Chicago Center for HIV Elimination.Her research focuses on the development, implementation, and evaluation of interventionsdesigned to address inequities in HIV/AIDS, substance use, and mental health among sexualand gender minority communities of color and on developing interventions that leveragethe power of supportive relationships to effect change.
Previously focused on parent-based interventions, her current research leverages the relational and contextual features of social networks and allied health professionals to improve outcomes in thePrEP, HIV, and MOUD cascades of care. She is the MPI of three NIH-funded Hybrid Trials designed to improve Continuumof Care outcomes among adults at risk for and living with HIV. She has served as the Co-Director of the Behavioral, Social, and Implementation Sciences Core of the Third Coast Center for AIDS Research, and is currently the Visiting Faculty Mentor at the Center for AIDS Prevention Studies at the University of California San Francisco. She mentors early-stage investigators and early career faculty on NIH awards.

Alida M. Bouris, PHD, MSW
The 21st Century Health Workforce
In partnership with Morgan Health
September 18, 2025 | 9am – 12pm
This convening will address health care challenges and avenues for workforce improvement. Key themes will include the current state of the U.S. health workforce, the urgent need to expand primary care capacity, scope of practice limitations, women’s health, and the return on investment of investing in a robust care workforce. Beginning at 9am, the hybrid in-person/virtual event will feature a plenary panel moderated by nursing professor and IPS Executive Director, Vincent Guilamo-Ramos, PhD, RN, FAAN, Leona B. Carpenter Chair in Health Equity and Social Determinants of Health.

Together, panelists will examine the economic imperative of diversifying the health workforce and how the nurse-driven model of care—working in partnership with community health workers and communities—optimizes the integration of clinical and social care. The event will also feature insights from JPMorganChase, the Federal Reserve Bank of New York, Oregon Health and Science University, Rhia Ventures, American Association of Nurse Practitioners, American Academy of Physician Associates, and the National Partnership for Women and Families.
June 4, 2025 – METHODOLOGICAL WORKSHOPS & NIH GRANT DEVELOPMENT
Marya Gwadz, PhD is Associate Dean for Research, Professor, and Director ofthe Intervention Innovations Team Lab (IIT-Lab) at NYU Silver. She also serves asan Associate Director in the Transdisciplinary Research Methods Core in theNIDA-funded Center for Drug Use and HIV Research (CDUHR) at NYU School ofGlobal Public Health.The main focus of Dr. Gwadz’s research is the development and evaluation of potent, innovative, and culturally salient social/behavioral interventions to address racial/ethnic, socioeconomic, and gender inequity in health. Dr. Gwadz is an expert on the multiphase optimization strategy (MOST), a framework for developing efficient and cost-effective interventions with no inactive, poorly performing, or counter-productive elements.

Marya Gwadz, PhD
May 21, 2025 – STRENGTHENING YOUR RESEARCH APPROACH: EXPERIMENTAL DESIGNS
Dr. Torsten B. Neilands is a Professor at the UCSF Division of Prevention Science in theDepartment of Medicine at UCSF. Originally trained as a social and quantitativepsychologist, he spent eight years as a statistical consultant at the University of Texasacademic computing center before coming to UCSF in 2001. Since arriving at UCSF, he hasparticipated as a statistical co-investigator or consultant on over 100 NIH, CDC, and stateprojects in the areas of HIV prevention, reproductive health, aging research, and tobaccouse prevention. His methodological areas of interest are multivariate statistical modelswith a special interest in latent variable models for survey scale development andvalidation as well as mixed effects (i.e., multilevel; HLM) models for clustered and longitudinal data, including dyadic data. His substantive interests include training the next generation of prevention researchers working in U.S. communities disproportionately affected by chronic diseases, including HIV and aging-related conditions. He is currently PI of two NIH-sponsored R25 research education grants to foster grant-writing and related research capacity-building for early-career faculty working in U.S. communities disproportionately impacted by HIV and STIs to prevent the spread of HIV/AIDS and STIs and to improve the lives of those living with HIV/AIDS. He also actively collaborates as a senior statistician and quantitative methods co-investigator on multiple prevention researchprojects. He is a co-author of Primer of Applied Regression & Analysis of Variance withDrs. Stanton Glantz and Bryan Slinker (McGraw-Hill, 2016).

Dr. Torsten B. Neilands
April 9, 2025 – DRAFTING INNOVATIVE AND IMPACTFUL SPECIFIC AIMS
AIMSAlida Bouris is an Associate Professor at the University of Chicago Crown Family School ofSocial Work, Policy, and Practice, and Co-Director of the Chicago Center for HIV Elimination.Her research focuses on the development, implementation, and evaluation of interventionsdesigned to address inequities in HIV/AIDS, substance use, and mental health among sexualand gender minority communities of color and on developing interventions that leveragethe power of supportive relationships to effect change.
Previously focused on parent-based interventions, her current research leverages the relational and contextual features of social networks and allied health professionals to improve outcomes in thePrEP, HIV, and MOUD cascades of care. She is the MPI of three NIH-funded Hybrid Trials designed to improve Continuumof Care outcomes among adults at risk for and living with HIV. She has served as the Co-Director of the Behavioral, Social, and Implementation Sciences Core of the Third Coast Center for AIDS Research, and is currently the Visiting Faculty Mentor at the Center for AIDS Prevention Studies at the University of California San Francisco. She mentors early-stage investigators and early career faculty on NIH awards.

Alida M. Bouris, PHD, MSW
Past IPS Convenings
IPS Convenings
The IPS Convenings series brings distinguished expert guests to the Institute for Policy Solutions to explore, illustrate, and amplify the transformative effects of employing a Nurse-Driven Model of Care to eliminate inequities in health care and health. Collectively, the series highlights the nine components of the Nurse-Driven Model of Care and how the model can reform our health care system by providing a mix of social and clinical care that ensures optimum health for everyone.
SPECIAL EVENT
Opportunities and pitfalls for health transformation in the new administration.
The Boundaries of Health: Debating the ROI of Programs and Policies that Integrate Social and Clinical Care

Vincent Guilamo-Ramos
Executive Director,
Institute for Policy Solutions

Kate McEvoy
Executive Director,
National Assoc. of Medicaid Directors

Chris Pope
Senior Fellow,
Manhattan Institute

Kody Kinsley
Former Secretary,
NC Dept. of HHS
The new Trump administration is pursuing intense transformation of how our government works. One of the administration’s stated goals, “Make America Healthy Again,” includes objectives that will require new thinking about preventing and treating chronic illnesses and eliminating health inequities. This dynamic panel discussion will debate the philosophical, financial and health implications of a reimagined health care system that pushes the boundaries of traditional care to include investments in mitigating harmful social determinants of health—an approach that has supporting and opposing views.
Support for an integration of social and clinical care argues that combining healthcare services with social support systems—such as housing, nutrition, and transportation—can lead to better health outcomes by treating patients holistically, while also reduce long-term healthcare costs by preventing chronic conditions, reducing hospital admissions, and promoting overall well-being. Opposing views, however, raise concerns about the logistical challenges, increased costs in the short-term, and the difficulty in coordinating diverse systems.
Don’t miss this timely debate featuring some of the leading thinkers on this topic.
How Nurses Can Drive Whole-Person Health and Eliminate Health Inequities within Medicaid
In the United States, the highly skilled and highly trusted nursing workforce constitutes the nation’s largest group of health care professionals. Leveraging the skills and scale of the nursing workforce can meaningfully advance whole-person health and health equity within Medicaid.
Join Vincent Guilamo-Ramos, PhD, MPH, LCSW, ANP-BC, PMHNP-BC, FAAN, Kody Kinsley, MPP, Linda Elam, PhD, MPH, and Megan Ingraham, MPH, MBA, for this exciting webinar exploring how to harness the nursing profession’s full potential by refining care models, addressing policy barriers, and fostering aligned payments.
This virtual event was recorded live on Thursday Dec. 12, 2024.

Vincent Guilamo-Ramos
Executive Director of The Institute for Policy Solutions and Professor at Johns Hopkins School of Nursing

Linda Elam
Managing Director, Manatt Health

Kody Kinsley
Secretary, North Carolina Department of Health and Human Services

Megan Ingraham
Managing Director, Manatt Health
Key topics will include:
- How a nurse-led model of care can address both clinical and social care to eliminate health and health care inequities in Medicaid
- Opportunities for optimizing the nursing workforce in strengthening the safety net
- Policy and financing recommendations that could support greater scale up of nurse-led care.
This discussion will build on a recent paper published in Nursing Outlook coauthored by several participating presenters which considered how the adoption of a nurse-led model of care can improve access to and quality of care for Medicaid members.