ABOUT THE
Cascading Disaster
A preventable and largely unaddressed public health emergency is accelerating. Only urgent, coordinated, multi-sector action can fix the failure.
What is a Cascading Disaster?

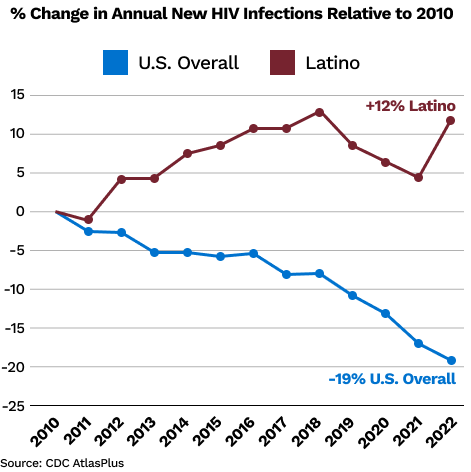
The HIV crisis among Latinos in the U.S. has worsened for more than a decade—even as the country overall has made major strides in reducing new infections and improving treatment outcomes. This widening gap is no accident: structural inequities in health promotion, testing, prevention, and care have gone unaddressed for years, fueled by “Latino invisibility,” discrimination, and damaging misperceptions about Latinos that have discouraged action.
Now, the Latino HIV crisis has become a cascading disaster.
Persistent inequities in our HIV response are driving higher infection rates, greater undiagnosed cases, delayed care, and poor viral suppression—which create a devastating cycle that continues to worsen the HIV crisis among Latinos.
Proposed cuts to HIV prevention and treatment funding would accelerate this downward spiral, making an already dire situation far worse. The longer this cascade continues, the more difficult and costly it will be to stop. A cascading disaster is a chain reaction triggered by a harmful event that spreads across interconnected systems, amplifying the harm at every subsequent step. Unlike simple cause-and-effect relationships, these harmful events escalate and worsen when stress in one system triggers failures in others. Often, the secondary effects are much worse than the original event.
In public health, cascading disasters are particularly hazardous because health, social, and political systems are closely intertwined. A breakdown in one area—such as access to care—quickly ripples outward, driving worse health outcomes, deepening economic losses, and destabilizing communities. Consider the COVID-19 pandemic, which led to a cascade of health crises, health system failures, economic disruptions, educational and social setbacks, and political polarization.
The Disaster at a Glance
While HIV outcomes have improved overall in the U.S., Latino communities have been left behind for years—and the gap continues to widen.
Systemic Neglect
Invisibility of the Latino community in the nation’s HIV response is a leading driver of the cascading disaster—fueling neglect and compounding inequities. Alongside invisibility, negative societal perceptions, stigma, medical mistrust, lack of health insurance coverage, and an insufficient public health response further intensify the crisis and make it increasingly difficult to reverse.

HIV progress in the US at risk of stalling—and Latinos face dire consequences
For several decades, the U.S. has made measurable progress in reducing new HIV infections and improving treatment outcomes through targeted investments in fighting HIV. Numerous federal initiatives—such as the ‘Ending the HIV Epidemic’ program—have expanded testing, broadened access to PrEP, and improved treatment, helping to drive national declines.
However, this progress is now in jeopardy. Changes in federal support and potential cuts to HIV prevention and treatment programs threaten to stall momentum—and even reverse course. For example, even a brief interruption to the Ryan White HIV/AIDS Program in the five cities with the most new HIV diagnoses among Latinos would lead to over 11,000 preventable new HIV infections by 2030, as estimated by a mathematical modeling study.6 If these setbacks occur, the consequences will reverberate across all communities.
For Latinos, a public health retreat on HIV poses especially grave risks. Even during times of national progress, Latinos have consistently lagged behind the U.S. population overall: facing higher infection rates, less access to PrEP, less treatment access, and poorer viral suppression. One example of why Latinos are faring worse is the fact that less than half of the Ending the HIV Epidemic initiative priority jurisdictions explicitly outlined strategies for engaging Latino MSM in HIV services in their local implementation plan, despite this group being disproportionately impacted by the epidemic.7 Reversing our HIV response would deepen these longstanding inequities that fuel the Latino crisis—and threaten the country’s ability to control and ultimately end the epidemic.
5 Forces Driving the Cascading Disaster
Continued failure to address these forces will not only deepen Latino HIV inequities but also undermine the nation’s overall HIV response.
1
Worsening HIV Incidence Inequities
While new HIV infections have decreased nationwide, they have increased among Latinos—who now represent one in three new cases. The crisis is even more severe for Latino MSM, who have seen sharp rises in new infections despite overall declines among MSM.
2
Persistent HIV Prevention & Treatment Inequities
Latinos at risk of HIV infection remain less likely to access PrEP than the overall US population of individuals who could benefit from PrEP, and Latinos living with HIV remain less likely to be aware of their status, access HIV care, or to achieve viral suppression than people with HIV in the U.S. overall. These inequities are driving preventable infections and avoidable illness, despite the lessons we have learned to improve HIV care outcomes for other groups.
3
Deepening Social Determinants of Health Inequities
Latinos are disproportionately exposed to harmful social and structural conditions, such as anti-immigrant policies, unstable housing, food insecurity, and overrepresentation in employment sectors with some of the lowest wages and fewest health care benefits—compounding barriers to HIV prevention and care.
4
Cuts to Latino-specific Federal and State Programs
Recent funding rollbacks have halted critical community programs and research that were addressing the needs of Latino communities and advancing efforts to end the epidemic. Medicaid cuts and widespread lack of insurance are pushing HIV services further out of reach for many Latinos.
5
Failure to Act and Prioritize Latinos
Despite the growing crisis, Latino communities continue to be sidelined in the national HIV response. This neglect is reinforced by damaging false narratives that downplay Latino contributions and obscure their disproportionate burden of the epidemic. Correcting these narratives is essential to mobilizing the societal and political will needed to end the cascading disaster.
The Latino HIV Cascading Disaster Affects Everyone
Building political will to end the Latino HIV crisis requires reframing the narrative. Latinos are not a marginal or external population—they are integral to the United States’ present and future. Eliminating HIV inequities among Latinos is an investment in the health, economic strength, and social well-being of the nation as a whole.
Correcting the False Latino Narrative
The Latino HIV crisis is exaccerbated by harmful myths that hurt health and progress. A common false idea is that Latinos are largely undocumented immigrants “taking” from the system. This stereotype not only stigmatizes Latino communities, but also distracts from the real issue: ongoing systemic inequities that not only drive the HIV crisis among Latinos but also make health outcomes worse for everyone.
Most Latinos are living in the U.S. without legal status.
Nearly 81% of Latinos in the United States are U.S. citizens—by birth or naturalization. There are also more than 1.5 million Latinos with legal permanent resident status (Green Card holders) in the U.S. Latinos are the second-largest racial/ethnic group in the country after Whites and Latinos are the primary driver of U.S. population growth. They represent more than 63 million people, projected to reach nearly 100 million, or 27% of the U.S. population, by 2060. Addressing the Latino HIV crisis is not about serving “outsiders”; it is about safeguarding the health of a vital and growing segment of the American population.
Latinos are a financial burden on the U.S. social welfare system.
Latino households and businesses generate more than $4 trillion in annual economic output. If measured independently, the U.S. Latino economy would rank as the fifth largest in the world—larger than the entire economies of countries like the United Kingdom, India, and France. Latinos are the backbone of the American workforce—in healthcare, education, construction, service industries, and agriculture. They serve in the U.S. military, hold elected office, and enrich the cultural and civic fabric of the nation.
Undocumented Immigrants Drain U.S. Health Care
Although undocumented immigrants represent only a small share of the U.S. Latino population, they contribute significantly, paying well over $50 billion each year in health insurance premiums and taxes that support the U.S. health care system. In fact, their contributions are five times greater than the health care dollars spent on their care. By contrast, U.S.-born citizens on average contribute less in premiums and taxes than the system spends on their behalf. In other words, the payments of undocumented immigrants subsidize the health care of U.S.-born citizens, helping sustain the system for everyone.
Latinos Lack Political Power
In the 2024 presidential election, a record 16.6 million Latinos cast ballots, the highest participation ever recorded and a decisive factor in several key states. The Latino electorate continues to expand rapidly, making it the second-largest voting bloc in the country. These indicators point to increasing Latino influence in shaping national and state policy priorities. Latinos’ growing political power makes eliminating their health inequities both an economic and political imperative.
The U.S. Latino Economy Ranks Among the World’s Largest
Latinos are powering one of the world’s largest economies — and America’s future.
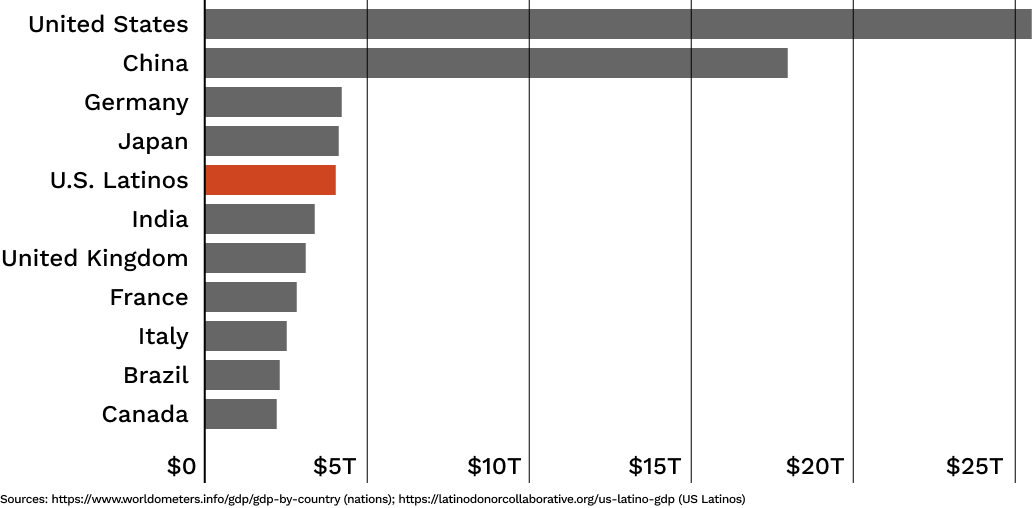
Latinos are not a burden to be managed—we are a force powering U.S. growth. To end the HIV cascading disaster, we must change the narrative, honor that value, and direct resources where they can transform both Latino lives and the nation’s health.Vincent Guilamo-Ramos, PhD, MPH, NP
Director, Center for Latino Adolescent and Family Health Leona B. Carpenter Chair in Health Equity and SDOH
Take Action
By prioritizing Latino visibility, strengthening prevention and treatment access, supporting community-led programs, and demanding political will, we can reverse these harms and move closer to ending HIV for everyone.
This page contains AI photographs generated by Midjourney.
- https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2018.304727
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10928966/
- https://www.cdc.gov/nchs/data/nhsr/nhsr107.pdf
- https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(24)00065-6/fulltext
- https://www.cdc.gov/mmwr/volumes/71/wr/mm7141a1.htm?s_cid=mm7141a1_w
- https://www.acpjournals.org/doi/10.7326/ANNALS-25-01737
- https://jamanetwork.com/journals/jama-health-forum/fullarticle/2838806