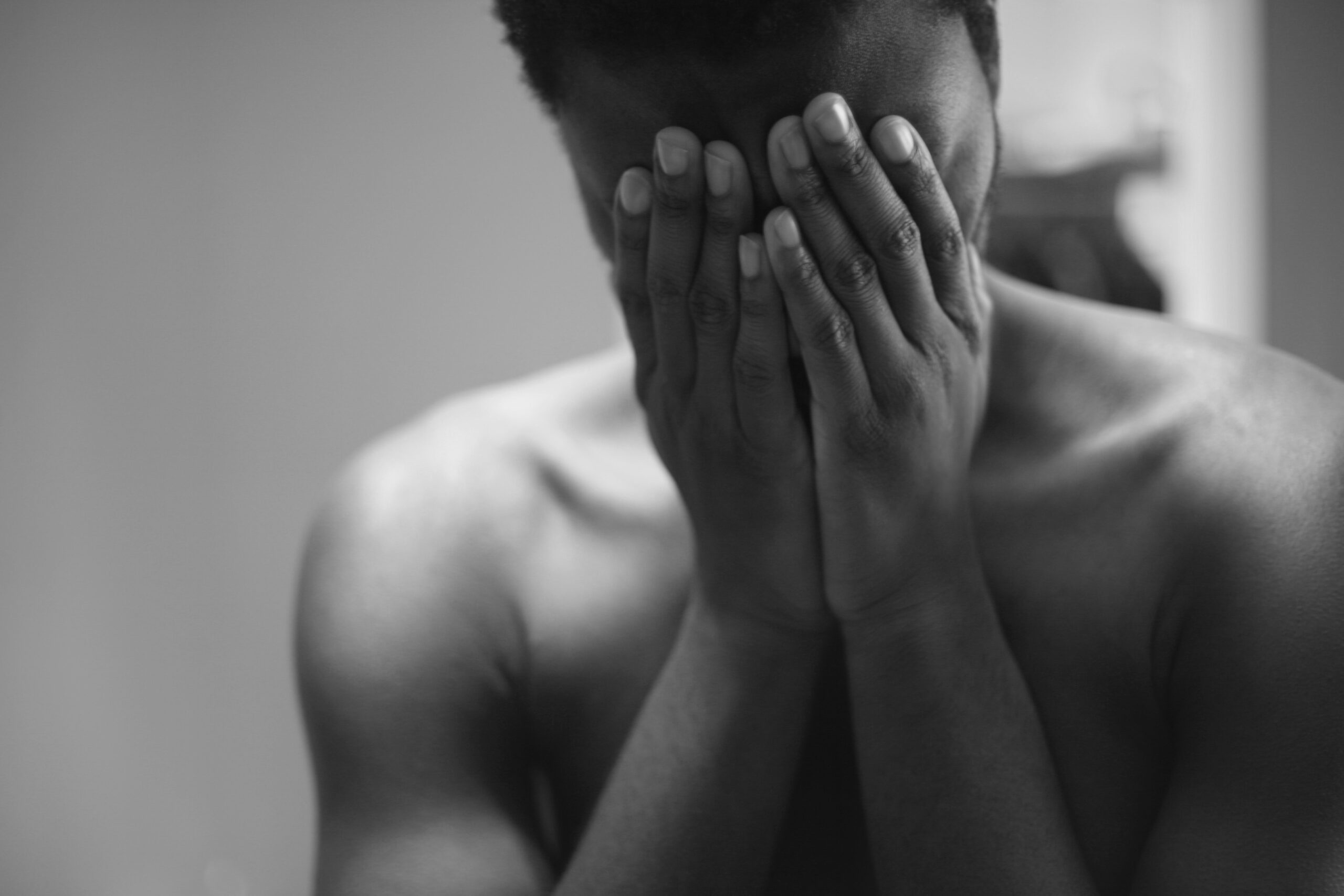
A young man with SCD presents to the ED reporting that his leg and back pain is a 9 on a 10-point scale. “Really?” The nurse responds in disbelief—he is not grimacing, sweating, or crying out in pain.
One of the first things that nurses learn about pain is that “pain is whatever the person experiencing it says it is.” Yet when individuals with sickle cell disease (SCD) present to the emergency department with reports of severe pain, they are frequently met with disbelief and their pain is often inadequately managed. In addition, most individuals with SCD are black (although the disease can affect individuals of any race or ethnicity) and many report experiencing racial discrimination during interactions with the health care system. In fact, race-based discrimination for patients with this disease contributes to negative provider attitudes, longer ED wait times, insufficient treatment, and lack of research funding.
What is sickle cell disease?
Sickle cell disease (SCD) describes a group of inherited blood disorders that often cause hard, sticky, and sickle or C-shaped red blood cells. SCD affects 90,000-100,000 Americans, affects millions globally, and although it is considered an African American disease in the United States, is the most common heritable blood disorder in the world. The most prevalent clinical complication of SCD is sickle cell crisis, an episode of severe, acute pain caused by occlusion of small blood vessels by the sickle-shaped cells. Sickle cell crises account for approximately 230,000 Emergency Department (ED) visits and over 1.5 billion in health expenditures annually. Despite the prevalence of sickle cell pain crisis, patients are often subjected to poor quality of care.
In the introductory narrative (from a scenario by William Zempsky, MD) a nurse’s implicit bias leads to unsatisfactory treatment for a young man in the midst of a SCD pain crisis. In these encounters, health care providers must recognize that SCD is a chronic painful condition with symptoms starting as early as 6 months of age. Over time, most patients with SCD have developed mechanisms to cope with severe pain that results in atypical, minimal, or non-existent objective displays of pain. That’s why it’s important for health care professionals to consider the psychosocial complexities of SCD—or any disease—when assessing a patient’s pain. Otherwise the subtle influence of stigma and implicit bias related to race and the disease itself can creep into care.
Unfortunately—and incorrectly— 63% of nurses believe addiction is prevalent among patients with SCD. Drug-seeking is a stigma often associated with sickle cell patients, but in reality patients with SCD are not more likely to misuse opioids than patients with other chronic painful conditions. Individuals with SCD experience multiple pain crises per year, and average 2-3 hospital visits per year. Each time, they become more familiar with what medications and doses work best with the least number of adverse effects. Unfortunately, requesting a specific medication and dose is considered a drug-seeking behavior, yet penalizing people for understanding their needs has resulted in 86% of SCD patients feeling that they are inadequately involved in decisions about their medical care. The drug-seeking stereotype also contributes to substantial delays in pain relief; 30% of nurses are reluctant to administer high-dose opioids.
Treatment guidelines published by the American Pain Society and the National Heart, Lung, and Blood Institute call for early and aggressive pharmacological treatment of sickle cell crises. These guidelines include an initial IV loading dose of short-acting opioid within 20 minutes of arrival at the emergency department (ED) and continuous reassessment and re-bolus every 30 minutes. In practice however, SCD patients have 25% longer wait times in the ED compared to the general patient population. It takes an average of 90 minutes, and sometimes up to several hours, for patients to receive pain medication. Moreover, providers are increasingly reluctant to provide opioids given the opioid epidemic. This puts health care providers in a tough spot, but we must check our biases and use our best judgment. Our patients must receive adequate pain relief when experiencing pain crisis; we cannot let patients suffer in our care.
Nurses have a critical role in improving pain management and quality of life. When assessing pain, believe the patient. When we doubt a patient-reported pain score, we should consider if our own implicit bias is impacting our clinical judgement. As we search for alternatives to opioids for moderate to severe pain treatment and develop new policy and practice guidelines, it is imperative that we keep in mind the unique needs of patients with SCD.
September is Pain Awareness Month, a time when various organizations work together to raise awareness of issues in pain and pain management.
This blog is a part of the “Dialogues in Health Equity” series by the Health Equity Faculty Interest Group. They are committed to decreasing health disparities experienced by local and global communities by promoting social justice and health equity through nursing practice, research, education, and service.
Dialogues in Health Equity
Pain Awareness Month

Helena Addison is currently a student in the MSN (Entry into Nursing) program, an executive board member of the Black Student Nurses Association, and a research co-coordinator on the Healthy Relationships Team led by Dr. Kamila Alexander. She plans to further her education by earning a DNP (Family Primary Care) and a PhD. Her interests include trauma, substance abuse, and health equity.