By Joan Cramer
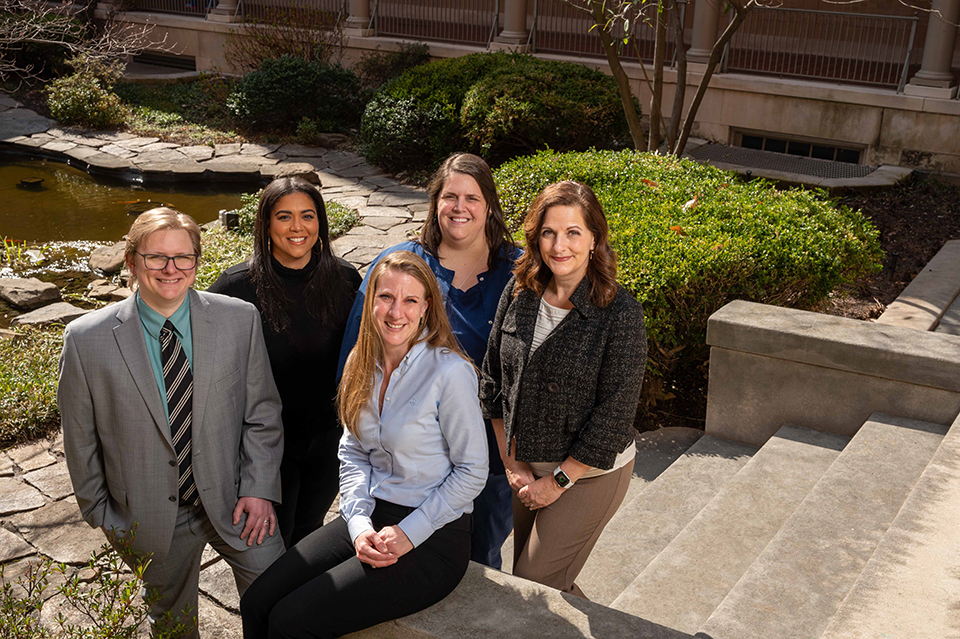
From left, Alex Tsikerdanos, Emily Batie, Katherine Pontone, Lucy Stewart, and Heather Watson of CORA.
In any hospital setting, some patients need constant observation. They might be disoriented or delirious, suicidal, aggressive, unable to communicate, or simply very young and can’t be left alone, so busy nurses often elicit the assistance of patient safety attendants (PSAs), to sit with those patients.
But as with many health care staffers today, PSAs are a scarce resource. Nurses at The Johns Hopkins Hospital who needed a PSA would call Intrastaff (the health system’s temporary staffing service) and negotiate for support. “The process wasn’t transparent, it was stressful and it could seem unfair,” says pediatric nurse educator Lucy Stewart.
Now, a PSA triage tool Stewart discovered in 2019—as a bedside nurse in the hospital’s pediatric anesthesia care unit working on her master’s degree in health systems management—has been adapted, tested, and fine-tuned, and is being used successfully throughout The Johns Hopkins Hospital. The constant observation resource assessment (CORA) is a tool nurses now use to put in a request for a PSA. It assesses each patient based on objective criteria and assigns a score based on the level of acuity or need.
Because PSA availability is still limited, nurses don’t always have their request filled, says Stewart. “But they know the process is objective and fair, and resources are being allocated where they are needed most.”
The CORA was based on a tool proven to work for brain rehab patients at Mayo Clinic, Stewart says. Katherine Pontone, nursing coordinator for the Department of Psychiatry and Behavioral Sciences, helped her adapt it to the specific needs of nurses and patients at The Johns Hopkins Hospital. At Stewart’s request, Heather Watson, a nurse scientist at Johns Hopkins Medicine’s Center for Nursing Inquiry, launched a research project with her team to test the reliability and validity of the tool. “You can’t just implement something and not find out first if it works,” Watson says.
In fact, over the past four years, more than 40 people have worked to bring the CORA to fruition, says Emily Batie, a project manager for the Department of Nursing who has helped coordinate the process. “There have been many moving parts,” Batie says.
When Stewart first proposed the tool, there was already a work group talking about the issue, which resulted in a community comprising stakeholders from every specialty. At the same time, the Department of Nursing created its own supplemental staffing unit, which took over the role of assigning PSAs (as well as nurses and clinical technicians who float across the hospital). And the hospital introduced a telesitter program, utilizing remote observers monitoring patients via screens from a centralized location.
“As changes happen, we are always refining the tool,” Batie says. She also says the Community couldn’t have done its work without Alex Tsikerdanos, now a Johns Hopkins University senior systems engineer, “who took all of our conceptions and put them into the software system OnBase. … Literally, the CORA was a piece of paper, and we’d sit around at meetings saying, ‘Where can we fax this?’”
Now, she says, the CORA has outgrown OnBase and is ready to be converted for use with the Johns Hopkins Epic medical records system. “It’s really a measure of our success,” Batie says. “And it means leadership will have access to the data and a real-time picture of our patient population to better meet our staffing needs.”
Watson’s team is continuing their research project, which was abruptly interrupted by COVID-19. “Change is slow and sometimes challenging,” she says. “But the tool has been shown to work.”
The next step, she says, is introducing the tool to the entire Johns Hopkins Health System. “We do a lot of collaboration with our six affiliates, and they know we have this tool, and they want it,” she says. “We’re just waiting for that final validity piece and then we can share it, which is super exciting. But none of this would have happened if a bedside nurse hadn’t introduced the idea.”