Told early on that he must choose between a career in either global public health or global clinical health—that the two paths didn’t really exist together—John Cranmer listened, then walked away even more determined.
“I was just beginning to learn what public health was, but I wanted to do it through a clinical lens,” he explains. “I thought, ‘Dang it, I’m just going to find a way to do it!’ ”
And so he has.
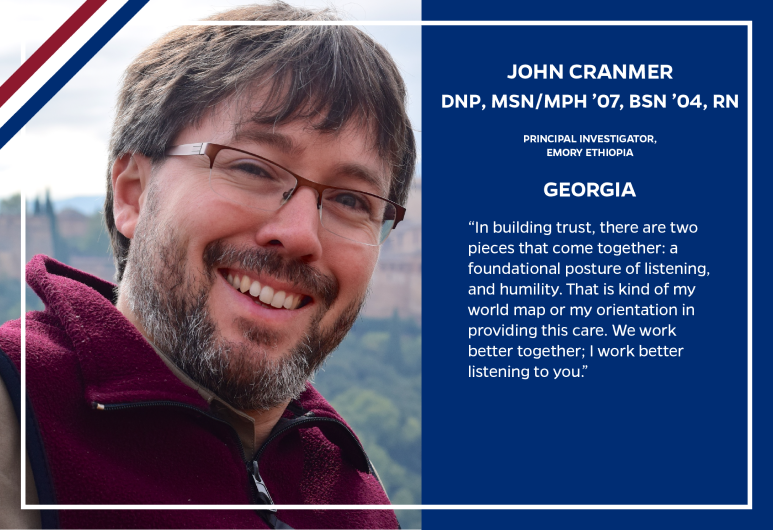
The associate professor at Emory University in Georgia and head of its Emory Ethiopia program, he found his skeleton key as part of the first cohort of the MSN/MPH program at the Johns Hopkins School of Nursing. (He later earned a DNP at the University Washington.)
Today, Cranmer is a global public health expert collaborating with governments, clinicians, communities, and scientists to address health needs with sustainable models of care in low- to middle-income countries. He has worked on solving maternal and newborn health issues in Kenya, Afghanistan and Ethiopia, where he also helped develop or fine-tune systems to address undernutrition among HIV populations. In Ethiopia, he has built upon the success of a program he worked with called Kangaroo Mother Care, which helps lower newborn deaths and build maternal bonds with newborns. He worked with a broad network of Ethiopian partners to design the Saving Little Lives initiative. This is a multi-agency, multi-national collective that brings lifesaving services to low-birthweight infants in Ethiopia.
Always, the most important piece is the community. And they key to it all, he says, is “collaborative practice.”
“In building trust, there are two pieces that come together: a foundational posture of listening, and humility. That is kind of my world map or my orientation in providing this care,” he says. “We work better together; I work better listening to you.”
He says it’s the same guiding principle he’s followed since starting as a clinical nurse practitioner in Baltimore and Washington state caring for vulnerable, non-native English-speaking communities. “My job was not to tell them what to do” but “to connect with them, to better understand them in their community context, and only then be a health adviser to them.”
At Emory, Cranmer designed and launched the Population Health track of its Doctor of Nursing Practice program before accepting the challenge to lead Emory Ethiopia, a position that put him on the ground in Ethiopia every few months among the team that he helped assemble and support.
For reasons of civil conflict and COVID-19, Cranmer has been unable to visit Ethiopia for two years. Yet the programs built have proven effective and sustainable, continuing to grow and thrive within the systems Cranmer and the collective designed. He takes great pride in that, but shares credit freely.
“That just speaks to the strength of our collaboration, and of the 50-plus staff we have across three regions of the country. Of course, when you’re immersed with your team you do the best work. We just had to pivot, learn different ways to work together, and we’ve done that.” — Steve St. Angelo
Click here to learn more about the programs at the Johns Hopkins School of Nursing.
Go to unitedstatesofnursing.org to see more stories in The United States of Nursing.