News from Around the World
Hopkins Nurses are Helping Haiti
Hopkins Nursing Center Offers E-Support to Nurses, Midwives in Haiti
Hands & Words Are Not For Hurting
Turning Health Education on Its Digital Head
Hopkins Nurses are Helping Haiti

On Jan. 13, 2010, Haiti experienced a 7.0 magnitude earthquake. The earthquake caused extreme devastation, hampering communication and relief efforts. A handful of Johns Hopkins nurses have made it their priority mission to help relieve Haiti.
Some have served in Haiti with the Johns Hopkins Go Team, a multi-disciplinary, stand-ready reserve of Johns Hopkins employees that can respond quickly to major catastrophes anywhere in the United States.
Assistant professor Elizabeth “Beth” Sloand, PhD, CRNP, has coordinated two more teams of Hopkins nurses to travel to grief-stricken Haiti with International Medical Corps (IMC). On March 5 and 12 IMC teams that included School of Nursing faculty members, graduate students, and alumni left for Haiti to provide medical care.
Read the blogs the nurses are keeping while in Haiti at www.nursing.jhu.edu/blogs/blogs/bsloand, www.nursing.jhu.edu/blogs/blogs/haiti and www.hopkins-in-haiti.blogspot.com.
Who’s been to Haiti?
Go Team
January 27 – February 10, Port-au-Prince
Marvin “Rocky” Cagle, RN (JHH)
Alicia Hernandez, RN (JHH)
Elizabeth Sloand, NP (JHU, faculty)
Go Team
January 26 – February 16, USNS Comfort
Meri Clare, RN (JHH)
Go Team
February 14 – February 25, USNS Comfort
Kathleen Feroli, NP (JHU)
Anthony Pho, RN, accel. ’08 (JHH and JHU, alum)
Sue Verrillo, MS ’03, RN (JHH and JHU, alum)
International Medical Corps
March 5 – March 21
Joyce Vazzano, MS, RN, CRNP (JHU, faculty)
Phyllis Mason, MS, RN, CANP (JHU, faculty)
Jennifer Stagl, RN (JHU, MSN student)
Rachel Klimmek, RN ’07 (JHU, alum and MSN student)
Tom Bernadzikowski, MS ’08, RN (JHU alum)
Michelle Felix, MSN ’95, RN ’93, CRNP (JHH and JHU, alum)
International Medical Corps
March 12 – March 28
Kathleen Becker, ANP (JHU, faculty)
Karen Gibbs, RN (JHU, MSN student)
Kristi Thane, RN, accel. ’07 (JHU, alum and MSN student)
The Waiting Game
Beth Sloand, Wednesday, January 20
As of Monday morning, members of the first group, Hopkins Go Team 1, have been briefed, vaccinated, and we are ready to go.
The Go Team leaders and administration are working around the clock to secure the logistics of the team. One top priority of any good relief team is to be sure that we are part of the solution and not add to the problem—of more mouths to feed and water, more needed shelter, more congestion in the already-overburdened country.
So we wait.
First day at Port-au-Prince University Hospital
Beth Sloand, Friday, January 29
We just finished our first day at the University Hospital. I spent a challenging day in the pediatric wards.
There are many children who needed care, but few people to deliver it. The supplies were difficult to come by; things were very confusing—with Swiss physicians, Haitian doctors and nurses, and us with our translators. The challenge is huge, with coordination, communication with various languages, cultural differences, etc.
One sad thing—there was a nursing school on the grounds of the University Hospital here. It collapsed. The bodies of many nursing students are still there—somewhere between 70 and 140. The bodies are entombed there. As a nurse educator, I am still struck every time I walk past that building. So very sad. Can’t get used to it.
First Day Realities in Haiti
Alicia Hernandez, Saturday, January 30

So much of this care involves deciding who to let die. The hard part means watching them die and watching their loved ones deal with their deaths.
Each death was different, each patient was different; from gunshot wounds from a riot, to [patients with] chronic illnesses sent from other hospitals, to Jane Does with no family, no identity, and who still hung on for hours with nothing left we could do. There is so much need, and so many people who want to provide, and so many obstacles.
And this is just our Day One. We will make a difference. I am determined. I don’t know how. I know even less so now than I thought I did three days ago. But with the good will and determination I sensed today, it will happen, no matter how slowly.
“Heartbreaking to see…”
Rocky Cagle, Tuesday, February 2
Today was another day in Haiti—hot. The Johns Hopkins crew is pretty much running the ER now with good outcomes.
We saw 470 patients today; others walked away. We see cases from tuber-culosis, malaria, typhoid, tetanus, gunshot wounds, motor vehicle accidents, CHF, etc. We are good at diagnosing these cases but there is a problem with medications; they are hard to come by.
We could save most of these patients with good facilities and meds. It’s heartbreaking to see people that we know are going to die without treatment that we can’t perform. Ten more days to make a difference in these peoples’ lives. If I only make one difference in one life, it will be worth this effort.
Home from Haiti, haunted by images
Beth Sloand, Saturday, February 13
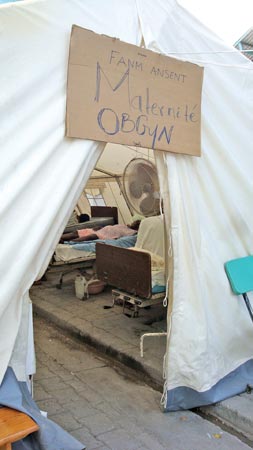
At the end of a visit, you leave Haiti. But Haiti doesn’t leave you. It has a way of clinging to your heart, never far away. This truth is even deeper in 2010, post-earthquake Haiti. Haiti haunts; it does not leave you alone. Memories are vivid: bandaged limbs of all sizes, odd surgical repairs, thick dust in the air as crews of Haitians sweep trash and shovel rubble, flies swarming wounds and IV bags in hospital wards that are open tents, patients limping from tent to latrine—holding tubing and bags of fluids, and more.
It was a great privilege to be in Haiti among so many relief workers from around the globe. We most certainly made a contribution. My translator Denise said, “Thank you for coming. Without you, many more people would have suffered and many more would have died. We are sorry that we have nothing to give you; we can only thank you. God will thank you.”
What’s Next?
Beth Sloand, Thursday, February 25
The school has been involved in Haiti for over ten years, and we have had 90-100 faculty and students visit in that time to participate in nursing education clinical experiences, clinical practice, and research. Now, post earthquake, we will continue our Haiti-related work with renewed energy in three major ways:
Awareness. We must keep the health and nursing needs of the Haitian population in the public eye. We are planning a panel discussion with Hopkins nurses who have been to Haiti for relief work. We are continuing the Hearts for Haiti campaign and keeping our Haiti web page up-to-date.
Fundraising. Funds raised by students, faculty, and staff will specifically benefit the two organizations that we have historically strong ties to: the Haitian Health Foundation and Haiti Nursing Foundation. To date, we have raised nearly $3,000, and we have several other events planned throughout March and April.
On-the-ground work. Faculty and students will continue to work in the Jérémie area, through our undergraduate PHN course and with graduate student and faculty participation in yearly multidisciplinary medical teams. Additionally, we will support the ongoing relief efforts in Port-au-Prince as opportunities arise.
Hopkins Nursing Center Offers E-Support to Nurses, Midwives in Haiti
In the aftermath of Haiti’s devastating earthquake, the Johns Hopkins University School of Nursing PAHO/WHO Collaborating Center has been actively assisting Haitian nurses and midwives from afar, gathering nursing education materials and making them available electronically.
As co-director of the Collaborating Center, Associate Professor Patricia Abbott, PhD, RN, manages the Global Alliance for Nursing and Midwifery (GANM), an electronic community of practice specifically designed to deliver information for nurses and midwives in low-resource settings. After the earthquake, the Center began an effort to collect nursing education materials, translate them into French and Creole and make them available to the nurses and midwives in Haiti electronically.
“We are getting educational material contributions for Haiti from some of the most desperately needy places in the world,” Abbott said. Materials have come from nations across the globe, including Japan, Afghanistan, Brazil, Pakistan, Nepal, and Somalia.
-Dave Alexander
How to Help Haiti

Students, faculty, and staff have launched a school-wide effort to raise money for two agencies with direct ties to the school. Both are nurse-focused and are already responding to the needs of the Haitian people since the earthquake.
Haitian Health Foundation
Jérémie, Haiti
Approximately 80 Hopkins nursing students and faculty have worked, learned, and served at the Haitian Health Foundation, an extensive community-oriented primary care system, over the past four years.
After the earthquake, Jérémie saw a massive migration of earthquake survivors who are pouring out of Port-au-Prince to outlying regions. Jérémie has already received over 200 people, many of whom are injured, all stunned and grieving.
Learn more at www.haitianhealthfoundation.org.
Haiti Nursing Foundation
Léogâne, Haiti
The Haiti Nursing Foundation (HNF) funds the first baccalaureate nursing school in the country, founded with the help of Alumna Ruth Barnard ’58, PhD.
With the school located in Léogâne, close to the epicenter of the earthquake, the dean, students, and a visiting nurse faculty volunteer “were mobilized within a half hour after the first quake. They set up 10 first aid stations around the town of Léogâne. Approximately 5,000 Léogâne townspeople are being cared for in the yard of the school. Six babies have been delivered by the Dean and students”
Learn more at http://haitinursing.org.
You can donate money to these foundations or to support our nursing students and faculty who travel to Haiti. Visit http://jhuson.givezooks.comand click on “Hopkins Nursing for Haiti.”
Hands & Words Are Not For Hurting
Hopkins nursing students address violence in St. Croix middle schools

The middle schoolers in St. Croix were still in shock and mourning. Just days before a group of Johns Hopkins nursing students arrived at their school, the young students had suffered a devastating loss—a teacher had been murdered by her partner.
The Hopkins students were there to deliver the message that “Hands & Words Are Not For Hurting,” and the timing of their presentation on nonviolence could not have been better.
The violence “comes from the neighborhoods and comes into the school and creates a problem for learning,” said Desiree Douglas, accelerated ’09. Douglas was among 15 Hopkins students and two faculty members who traveled to St. Croix in the U.S. Virgin Islands for the public health clinical rotation last summer.
On the itinerary was a stop at Elena Christian and Arthur Richards middle schools, both known to have a culture of violence including fighting and name-calling among the students. The Hopkins group presented The Hands & Words Are Not For Hurting Project, which allows participants to discuss violence and conflict resolution—and take a pledge to never use their hands or words to hurt others.
The Hopkins students spoke with more than 500 middle schoolers about the definitions of violence and examples of violent events on the island, allowing the young students to guide the conversation.
“As nurses [in the U.S.], we see that violence is our job, abuse is our job, and we should be dealing with it,” Douglas said. “The culture [in St. Croix] is different, but I think we initiated a conversation that needed to be happening. It seems as though they are opening to change.”
The program was so successful that the schools are planning to continue the program themselves. If sustained, The Hands Project may bring the St. Croix community more peace over time by helping make students aware of the power they have to stop the violence, Douglas said. “It starts with the students and teachers there,” she said. “That’s exactly what we wanted, and hopefully the students will continue.”
Learn more about the Hands & Words Project at www.handsproject.org.
-Sara Mitchell
Turning Health Education on Its Digital Head
Students use technology to share nursing knowledge around the globe
When Johns Hopkins University School of Nursing student Shehzin Mozammel began researching healthcare concerns in her native country of Bangladesh, she discovered that the country’s government is beginning to address HIV/AIDS, and figured that she could lend a hand.
“If there is one way I can give back, it’s a start,” she said. “I’m only one person, but I feel I can make an impact, even a revolution.”
Mozammel and four classmates in last semester’s Information Technology in Nursing course produced a slide show that outlines the disease’s spread among Bangladesh’s migrant workers and rickshaw drivers and offers basic information for healthcare workers and patients—even instructions for applying a condom.
The presentation is one of 10 group podcasts and narrated slide shows the class produced. Others address such health concerns as HIV/AIDS in South Africa, pediatric gastrointestinal disease and swine flu in China, and prenatal healthcare among Hispanic-American women. All take into account cultural sensitivities, with many narrated in the recipients’ languages.
For example, Holly Ohayon foresees her group’s Spanish-language slide show on improving nutrition and exercise among pregnant Hispanic Americans in Baltimore as usable in compact disc form. Either digital version represents “a new medium for people to obtain information,” she said.
The podcasts and slide shows are available digitally on the school’s Global Alliance for Nursing and Midwifery Electronic Community of Practice, a platform that allows medical professionals worldwide to exchange knowledge even under low-bandwidth conditions.
The students’ work reflects an evolution in the course, said Patricia Abbott, PhD, RN, FAAN, FACMI, co-director of the school’s Collaborating Center for Knowledge, Information Management, and Sharing.
“I just thought, ‘Let’s do a project that will benefit the outside world,'” she explained. “All of our students say, ‘I want to make a difference.’ [They] took this and flew with it.”
The experience of producing a digital education module “definitely is applicable to my future career as a nurse,” Mozammel said. The group’s project, she added, is both a resource for advancing health education among Bangladeshis and adaptable to reach patients elsewhere.
“As Bangladesh starts to move forward in technology, a simple PowerPoint presentation can be used to affect so many people,” Mozammel said.
Abbott is energized by the course’s digital turn. “The end users in any healthcare system will always be nurses, so [the students’] input will help create success in the future,” she said. “It comes down to new-world educating, and saying, ‘It’s not your mother’s nursing anymore.'”
-Hillel Kuttler
Urban Nurse, Village Doctor
Korean-American professor trains clinicians on China’s Korean border

In rural northern China, primary care is often provided by “village doctors” or “barefoot doctors,” practitioners with little formal training who rely on traditional methods and folk medicine for healing.
“We are taking the first step in building the infrastructure of community health workers there,” says professor Miyong Kim, PhD, RN, FAAN, who is translating her knowledge of community-based participatory research in Korean-American communities for use in China.
Li Chun Yu, PhD, RN, who once worked as a postdoctoral fellow under Kim’s mentorship, is coordinating efforts at Yanbian University to educate the village doctors and strengthen their capacity to serve their communities.
Last October, Kim traveled to Yanbian for a week-long training for village doctors. The focus: managing chronic diseases, especially for patients in rural settings. More than 50 healthcare providers attended the 2009 training, and more than 140 have been through the program since its inception.
Located near the Chinese-Korean border, Yambian is the only university in China that employs Korean and Chinese as official languages. This makes Kim a perfect fit for the program: She instructs her students in Korean or English, with a Chinese translator close at hand.
Kim plans to return this June for a week-long training on care for diabetes patients. Accompanying her will be three Hopkins nursing students, conducting research as part of the Minority Global Health Disparities Research Training Program. It’s just the beginning of a long partnership, as Kim and Li are seeking NIH funding to compare care for high blood pressure patients in U.S.-Korean and Chinese-Korean populations.
–Kelly Brooks-Staub