Losing a loved one became a teachable moment
By Kelly Brooks and Jodi Shaefer
The last evening Jodi Shaefer spent with her husband, Dave, he was feeling ill. Though he had been diagnosed with an inoperable brainstem lesion five years ago, there was nothing about his condition that night that seemed worth making a trip to the emergency room. The couple decided to wait through the night and visit the doctor in the morning.
That evening, though, he collapsed at home. He was rushed to the emergency room but could not be resuscitated. He died—surprisingly and unexpectedly—of a pulmonary embolism on March 10, 2010.
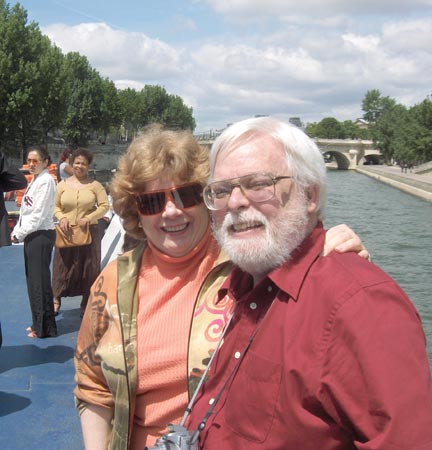
“I needed to see him to accept the reality of the death,” said Shaefer, PhD, RN, an assistant professor at the Johns Hopkins University School of Nursing. It was the first response to the grief and sadness after losing her husband of 34 years. “I wanted to stay with him while he was still warm. I just needed to sit and try to understand that Dave was dead.”
At 6:30 the next morning, she began calling family and friends. She then headed home, still in shock and disbelief, and contacted colleagues to help with her workload in the days to come. “It is part of who I am to cover my responsibilities and then deal with my overwhelming sadness and sense of loss,” she said. Everyone grieves differently; focusing on work was part of Shaefer’s way of handling the devastating loss.
Just over a week later, “still overwhelmed with the experience,” she wrote to her students and faculty colleagues: “I would like to tell you about Dave and how I am coping. It may give you some thoughts on dealing with patients as well as your own losses.”
In the months since her husband’s death, Shaefer has found that sharing her experience with others helped her to cope. She reminds us that it takes many months to years to learn to live with the loss of a loved one. Here, in her own words, is some of her advice for nurses working with the bereaved.
1. Be open and accepting to the needs of families, especially when they are in pain. Most families will remember your kindness, not the exact words you say.
2. Ask if there is anyone you can call for them. Friends or family? Transportation? Is there a phone in the room?
3. Offer food and drink.
4. Go into the room every 20-30 minutes. It is very isolating to be in the room, and it’s easy to feel forgotten. Sit for a minute and listen to them.
5. Ask whether they need a priest or other clergy. Make sure the unit or ED has this contact information.
6. Let the family know what will happen to the body and whether there are any papers to complete.
7. It is enough to say, “I am sorry for your loss. How can I help you?” The next challenge is to listen.
Coping Strategies
Find out how the grieving families you work with cope by asking, “Has anything like this ever happened before? How did you handle it?”Some healthy strategies include:
- Writing, journaling, or drawing
- Walking, exercise, or yoga (one father I worked with cut down trees)
- Listening to music or reading
- Talking about the event to friends, a mental health professional, or a minister
Also, do not forget to take care of yourself. As nurses, you need to have the emotional energy to care effectively for your patients. Develop your own healthy coping strategies and build them into your work schedule.
