By Elizabeth Heubeck
Photos by Whitney Sherman
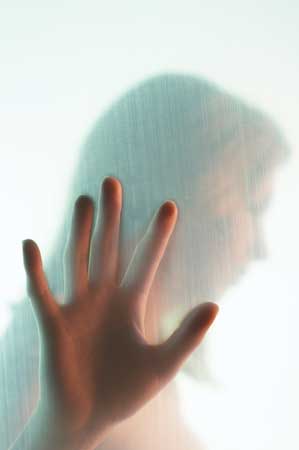
Hopkins Nurse are empowering women, throughout their lifespan, to embrace healthier
lifestyles

The birth of a baby. A diagnosis of breast cancer. The frailty that comes with old age. At the Johns Hopkins University School of Nursing (SON), students learn to perceive these and other health-related events as part of the dynamic, complex and ever-changing landscape that makes up a woman’s life span. They also are taught to recognize that the way these life events affect a woman have as much to do with where she grows up as what her genetic makeup looks like.
By looking below the surface at the important yet oft-overlooked subtexts that color women’s health, SON faculty members provide exemplary examples of how intuitive, targeted care leads to the best outcomes for every patient. They do so through the research they conduct, the evidence-based practice guidelines they construct, and the curriculum they design that speak to the health of all women at every phase of life. In turn, they empower the students they teach to practice nursing in a way that benefits the ethnically and socioeconomically diverse populations they serve.
The Early Years
Stemming the Rising Tide of STDs
A stint as a high school nurse steered the career path of Hayley Mark, PhD, MPH, RN, an assistant professor with the School of Nursing’s Department of Community Public Health. Stunned by the high rates of STDs among the adolescents she worked with, Mark wanted to find a way to reverse it. Subsequently, she has dedicated much of her career to researching ways to improve the prevention, spread, and treatment of STDs among young adults.

“One in every four teenage women has at least one STD,” such as human papillomavirus (HPV), chlamydia, herpes simplex virus, and trichomoniasis, says Mark. The rate of infection among African American young women is even higher, at 48 percent. While more intense screening would seem like a logical part of the solution, Mark has found it to be fraught with barriers.
For example, in a recent study, Mark and colleagues found that screening college students for herpes comes with its own particular set of challenges: the frequency of false-positive results; the expense—approximately $100—of confirmation testing; and the psychological repercussions among students who test positive.
Though nurses may not be able to change the nature or cost of screening for herpes, they can tune into the psychological repercussions that often plague young women who test positive for herpes and other STDs. “Nurses are often in the best position to help patients cope with the psychosocial issues involves,” says Mark.
Better Birthing With Doula Care
After she completed her clinical rotation in obstetrics, Suzette Lee ‘09 knew she wanted to be trained as a doula.

“Through my OB rotation, I became convinced that not all mothers-to-be are equipped to ask all the questions and request all the things they have the right to request,” Lee says.
Via a two-credit elective, SON students working toward their baccalaureate degrees can be trained as doulas—professionals who provide non-medical, emotional, informational, and physical support to women during low-risk childbirth experiences. Currently, about 15 percent of the program’s students opt to take the course. That’s a high percentage of nursing students choosing to learn age-old techniques that lie outside the realm of modern medicine.
Today, labor care in hospitals heavily emphasizes reducing pain, primarily via epidural anesthesia. This pharmacologic intervention isn’t without downsides. It necessitates an intravenous line; weakens women’s legs, making it difficult to get out of bed or effectively push during labor; and prolongs labor. By contrast, doulas use complementary comfort measures and support women’s choices during labor. But misperceptions have unjustly dampened the reputation of doulas.
“The hippie midwife/doula—that’s a myth. Those who are educated are very competent practitioners,” says assistant professor Elizabeth Jordan, DNSc, RNC, who runs the school’s Birth Companions Program with instructor Shirley Van Zandt, MS, RN, MPH, CRNP.
A free service, the Birth Companion Program pairs SON students who have received doula training with pregnant women in the Baltimore metropolitan area who lack a strong support system or access to prenatal care. The student-doulas provide clients with one prenatal and postpartum visit, and attend their labor and birth. The decade-old program, which currently serves approximately 75 women per year, has been collecting some compelling data on the women it serves.
“At a time when cesarean section rates are soaring, the rate for the women in the program is 5 percent lower than that in the community. Plus, the incidence of low birth rate and preterm infants is much lower than in the general population, despite the fact that we serve a vulnerable population,” Jordan says. Chances are it has something to do with the relationships mothers-to-be form with their doulas.
The Middle Years
When Mom Suffers Mental Illness
Motherhood doesn’t come with a manual. Even if it did, chances are it wouldn’t address the societal stresses that impinge on the life-long job: financial strain, an inadequate social support system, and addiction, to name a few. So countless mothers muddle through the job, feeling somewhat powerless and dragging down their children with them.
“When a mother’s mental health is impaired in any way, there are at least two people involved,” says Deborah Gross, DNSc, RN, FAAN, Leonard and Helen Stulman Professor in Mental Health and Psychiatric Nursing.
So Gross set out to develop a parenting program that would have a positive impact on both moms and their children. She chose to focus on a population that had been overlooked in prior data-driven parenting programs: urban Latino and African American families in Chicago neighborhoods. In addition to the challenges that all parents face, a large percentage of this population confronts additional burdens, including economic stress; violence, either domestic or neighborhood-based; and sparse or nonexistent support systems.
Gross, in collaboration with an advisory group of African American and Latino parents, developed The Chicago Parent Program (CPP). It emphasizes:
• Child-centered time
• The importance of family routines and traditions
• The value of praise and encouragement
• Rewards for reducing challenging behavior
• The importance of setting clear limits and following through
• The need to establish consequences
• The use of specific parenting strategies (e.g., ignore, distract, time out)
Gross’s program has met with success. Participants enrolled in the program for a year report using less corporal punishment, issuing fewer commands, and exhibiting more consistent discipline and warmth toward their children. Already, CPP has taken hold in Chicago, and Gross hopes to expand it into Baltimore soon.
But not all mothers who show signs of depression are enrolled in positive parenting classes, and it’s up to nurses to reach them in other ways.
“We may not always focus on the parents when we help their kids. However, clinicians need to take a step back and see holistically what’s going on with the mom, to be on the lookout for the possibility of mental health issues,” says Shelly Eisbach, a post-doctoral fellow who looks to Gross as her mentor in mental health research. She also assists staff at an intensive outpatient treatment center at Johns Hopkins Bayview Medical Center.
Staffing shortages and time constraints force providers to be creative when checking on moms’ mental health status. An increasing number of pediatric providers are conducting quick mental health screenings of mothers who bring their children to the office for care. “You have to look for opportunities to check in with moms. If you’re a nurse taking someone’s blood pressure, that could be the perfect time to communicate,” Eisbach suggests.
Heart Health First

We’ve all heard the refrain before: Girls are raised to take care of everybody but themselves. The negative consequences of this cultural norm—including cardiovascular disease, diabetes, and obesity—start to become apparent around the time women reach middle age.
Faculty members at the SON are working hard to change these cultural patterns, long embedded in communities, and to get women to take care of themselves first and foremost. For Deborah Jones, PhD, RN, and Hae-Ra Han, PhD, RN, it’s as much a professional initiative as it is a personal crusade, as they conduct heart health research within their own minority communities.
Jones, a SON assistant professor, lost her grandmother to heart disease, and she believes her grandmother—like many other African American women—lacked an awareness of risk factors that disproportionately affect a high percentage of African American women. She refers to them as the “deadly quartet”: obesity, hypertension, diabetes, and high triglyceride levels. And she’s determined to see make these disparities disappear.
Jones believes that breaking down barriers to improved health among African American women will require motivation and modeling. “If you sit down and show women what’s actually happening to them, it can motivate them to change. But don’t tell them; motivate them,” Jones says. “In the past, we tried to tell people what to do. It caused more resistance than assistance.”
The same may be true for Korean American women, who often consider their children’s success a stronger motivation than their own health. It’s just one example of how understanding a community’s culture is essential to communicating about lifestyle modifications.
“Korean American women want their children to go to the Ivies [Ivy League colleges],” says SON associate professor Han. “So instead of spending time and money on themselves, they spend it on their children. Their health is not their priority.”
Compounding this problem, explains Han, is the fact that many Korean Americans are small business owners, for whom private health insurance is extremely expensive. Conversely, Korea offers universal health coverage to its citizens. These factors, coupled with language barriers and an American health system that differs greatly from the one they’re accustomed to in Korea, prevent Korean American women from regularly seeing a provider.
Han’s research into hypertension prevention programs targeting Korean Americans reveals that using linguistically- and culturally-appropriate programs which emphasize lifestyle modifications can improve patients’ health outcomes. “We say, ‘Mothers are the backbone of society. You’ve got to be healthy for your dependent family members,’” she says.
The Later Years
Caring For Our Aging Population

Accompanying her great aunt to disappointing doctor appointments motivated Katherine Woodward ‘09 to enter the field of nursing. “Even with me there, she had a hard time speaking up for herself. And she forgot most of what she wanted to say. It’s a problem that’s too prevalent,” Woodward says.
Woodward is one of the 10 percent of SON nursing students who belong to the Geriatric Interest Group (GIG), a student-centered special interest group that addresses issues of special significance to older patients. The GIG hosts expert gerontology guest speakers and performs service projects within the community.
“We’re trying to prepare every nurse who graduates from the SON to care for the aging population. We’re committed to this,” says SON assistant professor Elizabeth “Ibby” Tanner, PhD, MS, RN, who originally formed the GIG in response to student requests.
With a host of other experts, Tanner developed curriculum for a course required by all SON baccalaureate degree-seeking students, “Issues in Aging,” which Woodward describes as “a great introduction to caring for older adults.” Only 23 percent of baccalaureate nursing programs nationwide offer a stand-alone required course in geriatrics, though one in every five American adults will be 65 or older by the year 2030.
This past winter, student GIG members threw an intergenerational “senior prom” for residents of a senior housing complex in Baltimore city, enjoyed by older residents and students alike. “It’s a misperception that all health care happens in a doctor’s office. Social interaction is therapeutic in its own right,” says Woodward, who attended the event.
The prom attendees offer proof. “One older person said to me, ‘I never knew I could have so much fun,’” Woodward says.
How Stress Takes its Toll
Though she admits it isn’t easy to pinpoint the link between stress and poor health, SON assistant professor Sarah L. Szanton, PhD, CRNP is determined to find the connection. Currently, she’s zeroing in on the impact of stress at the cellular level on older adults’ immune, cardiovascular, and endocrine systems.
“Oxidative stress may be the common soil for many things, from diabetes to cardiovascular disease. If we find more evidence of this, it could lead to findings on why some people age earlier,” Szanton says.
Already, Szanton’s research has identified links between older women’s stress levels and their health. A study revealed that community-dwelling women ages 70 to 79 who reported financial strain were almost 60 percent more likely to die within five years than subjects who reported no financial strain.
Armed with the knowledge that stress can adversely affect women’s health, Szanton believes it’s up to nurses to detect and find simple ways to help manage it. “It’s not your traditional nursing role. But it is a nurse’s business to find out about these things,” she says.
Surviving Breast Cancer
More than half of breast cancers occur in women over 65, but not all older women diagnosed with breast cancer have the same mortality rates. Women of certain ethnicities have less favorable survivor rates. SON faculty members are committed to leveling these statistics so that that all women, regardless of their ethnicity, receive culturally competent care that leads to the best possible outcomes.

Fannie Gaston-Johansson, PhD, RN, FAAN is painfully aware that the mortality rate for African American women with breast cancer is 32 percent higher than for Caucasian women. Gaston-Johansson, the director of the SON Center on Health Disparities Research, is finding innovative ways to change that disparity. She has discovered that spirituality and faith—cultural beliefs of great significance to many women in the African American community—can have a positive impact on the physical and emotional well being of African American breast cancer patients during treatment. She now suggests that nurses integrate spiritual and faith-oriented coping strategies as part of comprehensive breast cancer treatment plans for women of diverse ethnic and racial backgrounds.
Similarly unsettling statistics are fueling the research of pre-doctoral SON fellow JingJing Shang, MSN. One is the rising incidence of breast cancer among Asian American women; the other is the disproportionately low rate of Korean American women who receive breast cancer screenings, which can reduce breast cancer mortality by 30 percent.
“In the Asian culture, it’s not acceptable to talk about ‘bad’ things, like cancer. Some Asians, especially the older generation, believe they’ll be discriminated against if people find out they have cancer. Others think it’s contagious,” says Shang. “Cultural beliefs play a big role.”
For all ethnic groups, however, the odds for surviving breast cancer have never been better than they are today. But for the clinicians who treat these survivors, a long-term treatment model still doesn’t exist. SON assistant professor Sharon Olsen, PhD, MS, RN, AOCN is working with Johns Hopkins Breast Center colleagues to change that.
“We’re focused on developing a plan of care that can be as standardized as possible, and communicated to community providers,” she says. Components of such a model would include evidence-based medical care, patient and primary care provider education, surveillance, screening and support mechanisms.”
Olsen believes nurses can play an integral role in this model. She envisions nurses working more closely with oncologists, and a greater number of primary care nurse prac-titioners working independently with breast cancer survivors, especially given the shortage of general practitioners. Ideally, Olsen believes nurses could play a much larger role in breast cancer care management from the beginning stages.
“There’s a whole trajectory of care that nurses can be responsible for, from diagnosis to long-term survivorship management. These are the pieces where nurses shine,” Olsen remarks.
Learn More Online
STD Control and Prevention:
• Centers for Disease Control and Prevention www.cdc.gov/std/treatment/default.htm
• American Social Health Association www.ashastd.org
Midwives and Doulas:
• American College of Nurse Midwives www.acnm.org
• DONA International www.dona.org
Mental Illness:
• National Alliance on Mental Health www.nami.org
• American Psychiatric Nurses Association www.apna.org
Heart Health:
• American Heart Association www.americanheart.org
• Center for Disease Control and Prevention www.cdc.gov/DHDSP
Aging and Geriatrics:
• The National Gerontological Nursing Association www.ngna.org
• The Geriatric Nursing Project www.aacn.nche.edu/Education/Hartford
Breast Cancer:
• American Society of Clinical Oncology www.asco.org
• Institute of Medicine Cancer Survivorship www.iom.edu
• Oncology Nursing Society www.ons.org
• Susan G. Komen for the Cure, Maryland www.komenMD.org