The hot new field of forensic nursing — equal parts detective work, medical know-how, and compassion — is taking off at Johns Hopkins, under the leadership of nurse-turned-crimefighter Dan Sheridan.
Story by Jeff Labrecque, A&S ’95
Photos by Keith Weller
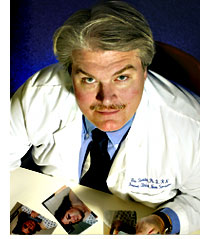
How are you at looking at gross things?” When Dan Sheridan asks you that question and reaches into a thick folder of graphic case photography, you’d better be prepared. Sheridan, PhD, RN, has built a career studying the impact of violence on the human body, and he’s developed quite an eye for it. “Injuries talk to me,” he says. “Any good forensic nurse learns very quickly to interpret what injuries are telling them.”
What those injuries actually say may answer some truly horrible questions. The rapidly-growing field of forensic nursing — one of the fastest-growing specialties in nursing today — is routinely involved with cases of sexual assault, domestic violence, child abuse and neglect, elder abuse, and other forms of traumatic violence. At the Johns Hopkins University School of Nursing, Daniel Sheridan is the architect of a new, 39-credit master’s specialty in forensic nursing aimed at preparing a new generation of leaders in the rapidly evolving field. “The forensic nurse needs to have a little bit of detective in him, to be able to do some deductive reasoning, and to be able to put all of the pieces together in order to solve a complete puzzle,” says Sheridan, who in addition to serving as an assistant professor at the
School of Nursing, is a forensic clinical nurse specialist at the Johns Hopkins Hospital, where he is working to establish forensic policies and procedures for medical personnel who treat suspected crime victims.
Considered one of the world’s leading authorities in forensic nursing, Sheridan was awarded the Virginia Lynch Pioneer Award in Forensic Nursing by the International Association of Forensic Nurses in November 2002, the highest award given by the association, and in December, he was chosen president-elect of the IAFN. Although the Johns Hopkins School of Nursing is not the first to include a forensic curriculum — it was the fourth, actually — the school’s national reputation and its decision to recruit Sheridan reflect the increased importance placed upon forensics.
“We have been looking at the health connections to violence for quite a while,” says Jacquelyn Campbell, PhD, RN, associate dean for faculty affairs and the school’s Anna D. Wolf Professor. “There’s been a real growth in the job market for this particular specialization, and people are starting to realize that we need to be doing much more training for nurses.” Campbell is pleased with the strength of the forensic nursing program now in place at the school. “Between [Dan’s] forensic expertise and our expertise on other aspects of violence and health,” she says, “we really have the cadre of faculty that can support this kind of specialization for our students.” Forensic nursing students can expect to take a variety of classes, ranging from Ethics of Health Care to Family Violence.

By definition, forensic nursing is the application of nursing when it overlaps with the legal system, but the fit is not always a smooth one. “Forensics is sometimes the collision between law and medicine,” Sheridan says. In the hospital emergency room, some physicians might be reluctant to welcome law enforcement officials onto their turf, and law enforcement can grow equally frustrated and impatient with hospital practices. Although the medical, legal, and social authorities are working together, “everyone’s focused on their own priorities,” Sheridan says. “The police, obviously, want evidence. We want to save a life.” In those efforts to save lives, doctors, nurses, and technicians might cut, taint, or discard a victim’s clothes — clothes that may be filled with evidence that can make or break a case.
Nurses are in an ideal position to bridge these worlds, according to Sheridan. “It’s easier to train a nurse in the principles of evidence collection and preservation and crime scene analysis than it is to train cops in health care principles,” Sheridan says. Obtaining accurate histories from crime survivors, for example, can be crucial to building a solid case. The empathy inherent to good nursing makes nurses particularly well-suited to this difficult, often emotion-filled, interviewing task.
Once the case moves into the courtroom, forensic nurses make valuable witnesses in legal proceedings. Prosecution and defense teams both recruit nurses to serve as expert consultants for their respective cases. In cases of elder abuse or neglect, for instance, attorneys might hire a forensic nurse to testify as to what is or should be a reasonable standard of care. Although some nurses are asked to make courtroom appearances, they are more commonly tapped to consult during pre-trial procedures, where the weight of their expertise may encourage a settlement and thereby avoid a trial.
Sheridan recently participated in just such as case. An Oregon couple had been suspected of negligence after an elderly family member died at home and was discovered to have gross discolorations on one side of her body. The local police believed the markings were the symptoms of abuse, but Sheridan came to a different conclusion after reviewing the evidence. With the exception of the bedsore-like wounds, there were no signs of neglect: the woman’s hair was clean and her fingernails were neatly trimmed. A little research revealed that the dying woman was suffering from peripheral vascular disease, an arterial ailment that caused the suspicious-looking discolorations, and Sheridan urged the authorities to halt their investigation. “Forensic nurses cannot only help put bad guys in jail,” Sheridan says. “We can get innocent folks out.”
Not all of Sheridan’s cases end so neatly. As an operation room scrub technician in the Air Force in 1975, he saw a woman who had been methodically shot five times — once in each arm, once in each leg, and once in the stomach — by her husband, who had suspected she had been unfaithful. The case was an appropriate introduction to the growing problem that Sheridan would spend his career fighting: domestic violence. In 1978, he volunteered at a battered women’s hotline — founded by a handful of women, including his wife, Marge — which evolved into a battered women’s shelter. In 1986, a few months after finishing his master’s degree at Rush University in Chicago, Sheridan set up the second hospital-based family intervention program in the country. “I had figured out by 1986 that family violence was not something that just affected women,” Sheridan says. “It affected kids, and if there were elderly in the home, it affected them. It affected everyone.”
But forensic nursing, at least officially, did not exist at the time. “I didn’t know I was doing ‘forensic nursing’ until about 1991,” Sheridan says, and it wasn’t until 1995 that the American Nurses Association officially recognized forensics as a nursing specialty. Lacking any real guidelines, Sheridan and other forensic pioneers working with rape victims and battered women developed their own training and procedures — often independent of each other. “I was able to manipulate just about every course requirement in my undergraduate and graduate degrees to do something in the area of family violence,” Sheridan says. Even as a student at Rush, his two years of experience with the battered women’s hotline made him the most qualified person on that subject at the school.
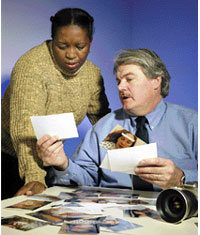
Sheridan’s arrival at Johns Hopkins coincides not only with increased demand for forensic specialists but with increased interest among nursing students. Since 1995, IAFN membership has jumped more than 400 percent. At Hopkins, there are currently 10 students pursuing the graduate forensic focus, a number that promises to grow quickly given the high level of interest expressed by applicants to the school. One nursing student is Sine Duma, who came all the way from South Africa after hearing about the program from School of Nursing dean Martha Hill during her 2001 visit to that country. Says Duma, “She told me about the course and about Dr. Sheridan, and then we started talking by email, and hence, I’m here.” Duma, a faculty member at the University of Cape Town, came to Johns Hopkins to develop a research proposal on domestic violence for her doctoral studies in South Africa.
There are 33 other students (both undergraduate and graduate) enrolled this semester in Sheridan’s Fundamentals of Forensic Nursing class. One of them is Nancy Gruber. “I’ve always found the field interesting just from seeing different shows on TV,” says Gruber. Those shows include CSI: Crime Scene Investigation, a popular CBS drama series about a team of experts who use forensic techniques to solve crimes. The show has been criticized for favoring fiction over forensics — it’s “about 5 percent reality, 95 percent Hollywood,” according to Sheridan — and Sheridan jokingly warns his students: “There is absolutely nothing on CSI that will help you pass this class.”
A tolerance for the intolerable will help, though. Paging through the suggested readings at the first class, students could find police photos of Jeffrey Dahmer’s victims, among other grisly images. “If you think looking through these books is cool instead of gross,” Sheridan told his students, “you have the aptitude to be a forensic nurse.” Forensic nurses are required to work amidst significant disfiguring trauma and ugly social histories, and Sheridan stresses to his students that they will need to maintain a strict sense of objectivity. “The worst thing in the world that you can do as a forensic nurse is to chart in a way that someone who reads your notes knows that you’re angry, that you’re upset, that you’re frustrated,” Sheridan says. “A defense attorney can easily demonstrate that a forensic nurse is pro-victim, simply based on the words that appear on a chart.”
Those who complete the forensic master’s program will be uniquely qualified for a wide variety of nursing positions. There is currently a great need for forensics experts to coordinate sexual assault nursing examiner centers at hospitals and clinics, where thorough and timely examinations are the difference between a rape conviction and an acquittal. “The sexual assault examination is a gathering of evidence kind of procedure, but it’s also a health assessment,” says Campbell, emphasizing the dual roles that nurses provide. “If it’s done from a nursing perspective, it can also provide the kind of emotional support that a sexual assault victim so badly needs.”
Forensic skills are also valuable on death investigation teams, child and adult protective services, and family violence emergency room intervention programs. In the ER in particular, knowledge of forensic principles is becoming increasingly essential, says Marian Grant ’00 a staff nurse in the Adult Emergency Department at Johns Hopkins Hospital, who attended one of Sheridan’s staff education seminars. “Even though I was taught about domestic violence in school, his instruction to us has been helpful because now I find myself asking patients more questions,” says Grant, who is currently pursuing a graduate degree at the school. “A lot of these patients slip through the medical system because no one asks them the hard questions, and it’s a lost opportunity for us to help them.”
Sheridan’s staff education seminars are just the first step in a coordinated effort — an effort he is leading — to institute uniform forensic policies and procedures for abuse victims at Johns Hopkins Hospital. Rather than being the expert who is always called in on cases of suspected abuse, he is working, he says, “to get the staff to be the ones who are providing a minimal standard of forensic care.”
Sheridan’s recommendations have already made an impact on the Department of Emergency Medicine, and the hospital is on the verge of implementing new procedures and protocol for evidence collection and wound identification and documentation. Sheridan has worked closely with hospital administrators and practitioners to make sure that new policy is acceptable and practical for everyone. “This sort of systems change isn’t something you can come in and tell people you need to start doing this tomorrow,” he says. “If you really want it to work, you have to have the support and collaboration of the people who are going to have to do the work.”

Johns Hopkins Hospital is committed to improving its overall forensic response, and the School of Nursing is dedicated to becoming the international leader in forensic nursing education. Sheridan’s supporters say he is the right person to lead both efforts. “Dan has this wonderful combination of a background in mental health and in emergency department care,” says Campbell, who has known Sheridan since 1981. “Plus, he is a dynamite speaker and teacher, so he makes training in these issues come alive.”
Sheridan could not be happier to have landed at Johns Hopkins. “I used to say when I did a lot of training around the country that the only thing that would bring me back to academia would be the chance to set up a forensic master’s clinical specialist program,” he says. “So the moral of the story is, be careful what you wish for; sometimes it comes true.”
Jeff Labrecque writes from Baltimore.