Nursing the Wounds of War
by Teddi Fine
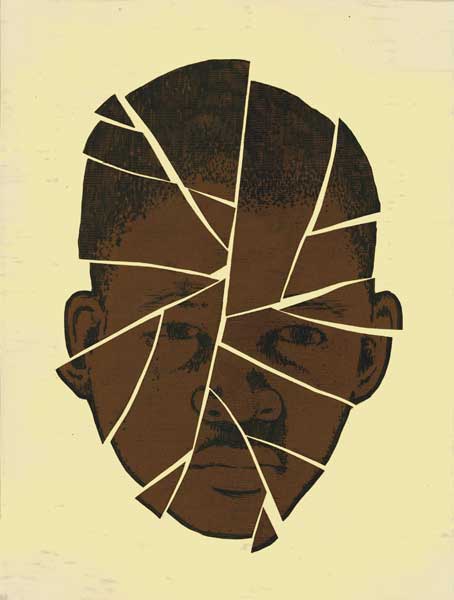
When a suicide bomb detonates or an improvised explosive device blows up at a roadside or in a car, the damage can be both vast and shattering for those nearby, whether the victims are soldiers or innocent bystanders. These explosions send shrapnel—sharp bits of metal—into everything and everyone near them. As seen in far too many news accounts of the combat in Iraq and Afghanistan, lives and limbs can be lost or shredded.
In many cases, shrapnel wounds are small, superficial, soft-tissue injuries that combat nurses and doctors call “peppering wounds.” They literally “pepper” a portion of the body—too often the face and neck—with these tiny wounds, frequently with bits of embedded metal.
While not among the life-threatening injuries seen in combat-zone med-icine, these potentially disfiguring wounds are among the most common, and the most susceptible to independent management by nursing staff. But, as Air Force Major and JHUSON graduate Jennifer J. Hatzfeld, PhD, RN, realized during her deployment to a military hospital in Kandahar, Afghanistan, no established guideline existed to support nursing assessment and treatment of these superficial shrapnel wounds.
Training varied markedly among the U.S. Navy-managed hospital’s inter-national nursing roster from across military services in the U.S., Canada, the Netherlands, and the United Kingdom. So Hatzfeld and a number of her colleagues at the Kandahar hospital took action.
The team mapped out a best-practice protocol for patients with peppering shrapnel wounds. They approached the issue from a common nursing perspective: focusing holistically on the needs of the individual patient and combining immediate and specific treatment protocols with attention to longer-term needs related to pain management, nutrition, and emotional support.
And all this despite responding to mass casualties in an environment of escalating operations and limited access to research resources and a dearth of research on the topic. The work was done between shifts, on precious days off, and in moments between patient care and the next crisis; but the work was done. The very process of creating the protocol had a tangible benefit by bringing together a diverse group of clinicians from different countries with different nursing experiences, all of whom were far from home and working under extreme circumstances.
Their accomplishment, observes Hatzfeld, is “a great example of what nursing teamwork is all about.”
Today, as director of nursing research at Travis Air Force Base in California, Hatzfeld notes, “This was a very small project dealing with an unfortunately common battlefield injury. Our work certainly does not revolutionize the already great care that’s being provided to our injured service members in the field, but it does have the potential to make caring for these wounds a bit easier, with more successful outcomes.”
The work she humbly describes as small may in fact have big applications closer to home. In the event of a disaster, the guidelines she helped craft could well give nurses the guidance they need to better care for patients with wounds they previously had never seen or treated.