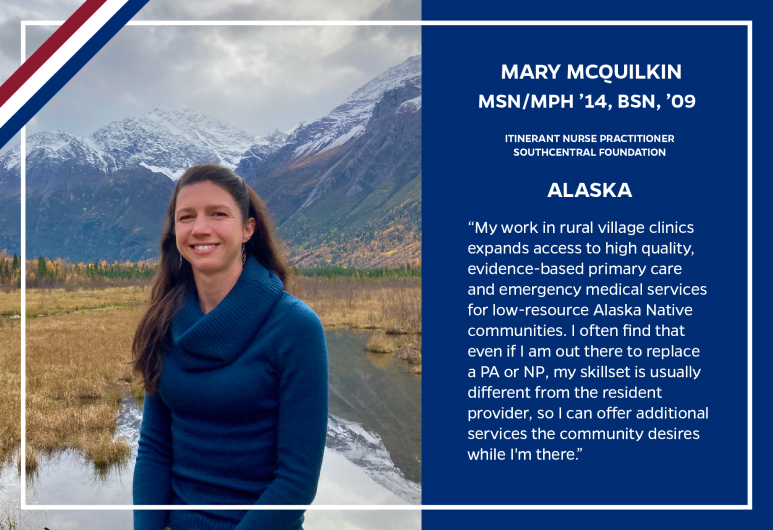
In a state larger than Texas, California, and Montana combined, access to healthcare can be a difficult thing to come by. Mary McQuilkin, NP, MPH, is one of the dedicated healthcare workers who quite literally brings healthcare to the Alaskan people.
Mary has to be prepared for anything in her role as an Itinerant Nurse Practitioner for the tribal health organizations of Alaska.
“When a clinic is short staffed, I fly out to the village on a small plane and work in the clinic to provide primary care and emergency medical services.”
That means that when someone calls 911 for a health emergency in a rural Alaskan village, Mary’s phone is the one that rings.
When Mary is heading out for an assignment, she usually has almost no information about where she is heading, just that her help is needed. And that’s all the information she needs.
Mary has always felt the call to help people. After completing her undergraduate degree, she embarked on a 4,000 mile cycling trip to fundraise for cancer research in Baltimore. Only two days after completing this trek, Mary hopped on a plane to Uganda to work as a United States Peace Corps Volunteer. While in Uganda, Mary helped educate the local population about HIV and ways to help prevent and mitigate the spread of the disease. She also taught them ways to utilize their crops better, so the locals could incorporate a more nutritious diet into their lives.
It is safe to say that Mary has always felt the urge to help those less fortunate and after returning to Baltimore, Mary made her way back to school to get her MSN-NP/MPH degrees.
Where better to put those credentials to work than in the unforgiving environment that is Alaska?
“There are 228 federally recognized tribes in Alaska, and Alaska Native people have a lower life expectancy and worse health outcomes across many metrics compared to the general U.S. population. Health disparities in Alaska Native people are due in part to structural challenges such as remote location with limited access to transportation and goods from outside the community. The nutrition of many families comes from subsistence hunting, fishing, and gathering berries seasonally. Getting fresh fruits and vegetables in a village most of the year is very difficult because some places only have a couple small planes come in per week, and those have very limited space onboard for cargo. This makes produce very expensive, and it may be old by the time it arrives. Meeting the recommendations for physical activity is also more challenging than in most of the lower 48; it gets -60˚F in one village where I worked recently, and there are no indoor recreation centers.”
When Mary gets called out to help at one of the tribal health clinics, she packs her bags with supplies and heads for where she is needed. Many of these communities do not have access to traditional resources which can make life a little difficult at times.
“Many villages don’t have a store or restaurant. If they do have a store, no normal person could afford to shop there (a colleague of mine found a small bag of chips for $8.50!). So, I pack minimal clothing and personal items but fill a duffel bag with 50 pounds of non-perishable food which can last me almost 3 weeks.”
Providing healthcare in Alaska takes a certain amount of determination. Determination that is clearly shown in Mary’s past and current work.
“In my role, I need to meet people where they are (both figuratively and literally by going there). I work with individuals on practical solutions to improve their health, taking into account both the challenges of their living situation and available resources that can be leveraged to achieve their health goals.”
Living and working in Alaska’s harsh environment does have some benefits too. Mary recently had the opportunity to work on St. Paul Island in the middle of the Bearing Sea, often referred to as “The Galapagos of Alaska.”
Click here to learn more about the programs at the Johns Hopkins School of Nursing.
Go to unitedstatesofnursing.org to see more stories in The United States of Nursing.